Research Article
Clinico-epidemiological characteristics and survival outcome of patients with hypertensive crisis at Kassala Hospital, Eastern Sudan

TajEldin M Abdallah1*, Abdalazeem A Ibrahem2, Ezeldein A Ali3, Elbashir G Ahmed1 and AbdelAziem A Ali4
1Department of Medicine, Faculty of Medicine, University of Kassala, Sudan
2Department of Cardiology, Yesbyty Gwynedd, UK
3Prince Sultan Military City, Riyadh
4Department of Obstetrics and Gynecology, Faculty of Medicine, University of Kassala, Sudan
*Address for Correspondence: TajEldin Mohammedein Abdallah, P.O. Box 496, Department of Medicine, Faculty of Medicine, Kassala University, Kassala, Sudan, Tel: +249912820929; Fax: +249411823501; Email: tajeldinmm@yahoo.com
Dates: Submitted: 22 October 2018; Approved: 30 October 2018; Published: 31 October 2018
How to cite this article: Abdallah TM, Ibrahem AA, Ali EA, Ahmed EG, Ali AA. Clinico-epidemiological characteristics and survival outcome of patients with hypertensive crisis at Kassala Hospital, Eastern Sudan. J Clin Intensive Care Med. 2018; 3: 029-034. DOI: 10.29328/journal.jcicm.1001017
Copyright License: © 2018 TajEldin M Abdallah, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hypertension; Crisis; Emergency; Urgency; Sudan
Abstract
Introduction: Hypertensive crisis (HC) is recognized consequence of inadequate blood pressure (BP) control. A hypertensive crisis is further divided into hypertensive emergency (HT-E) and hypertensive urgency (HT-U).
Method: Using a cross-sectional hospital-based study design, patients who had been diagnosed as having HC between January and October 2017 were consecutively recruited in the study. The criteria proposed by the Seventh Joint National Committee were used for the definition of HC.
Result: A total of 81 (.81%) patients newly diagnosed as having HC were enrolled in the study. Of these patients, 50 (61.7 %) patients met criteria for HT-E, while 31 (38.3%) patients had HT-U. Renal impairment (16%), stroke (30.8%), acute coronary syndrome (13.6%) and heart failure (22.2%) were predominant complications associated with HT-E. Out of 81 study subjects, 13 (16%) patients died. Although there was no significant difference in residence, history of smoking, Diabetes mellitus and history of alcohol consumption between groups, old age (P=.o22), male gender(.046), history of hypertension(.007), history of non-governmental employee(.003), poor compliance (p=.002) and high case fatality rate (p=.041) were significantly associated with hypertensive emergency (HT-E).
Conclusion: This study showed that HT-E has high case fatality rate among patients admitted with hypertensive crisis at kassala teaching Hospital. Therefore early detection of hypertension and appropriate management are the main stay for reducing morbidity and mortality among patients with hypertensive crisis.
Introduction
Hypertension is a major health problem nationwide that necessitate special emphasis. Hypertension is the third leading cause of death globally, and round seven million people die each year as a result of hypertension. In sub-Saharan Africa the prevalence of hypertension was estimated by 30% among general population. In the Eastern Mediterranean Region, the prevalence of hypertension was reported as 26% [1,2]. The prevalence of Hypertension among non-communicable diseases has been accounted for 23.6 % and 39.6% in central and Northern Sudan respectively [3,4]. Hypertension represents one of the 10 leading causes of death in Sudan and responsible for 1.3% of the outpatients visits [5].
It has been estimated that around 1% of patients with hypertension develop a hypertensive crisis during their lifetime, as consequence of inadequate blood pressure (BP) control. Hypertensive crisis (HC), is defined as extreme and symptomatic rising in BP (usually ⩾180/120 mm Hg). According to criteria proposed by the Seventh Joint National Committee HC was classified into either a hypertensive emergency (HT-E) or hypertensive urgency (HT-U) depending on evidence of target organ damage; HT-E is manifested by rapid worsening of target organs such as heart, brain, kidneys and arteries. HT-U is characterized by severe elevation of the blood pressure without evidence of end organ damage that need to be treated with oral anti-hypertensive drug, in order to reduce the BP within 24 hours [6-8].
Although HC is well described worldwide, there is no published data regarding the characteristics of individuals with HC in Sudan. Therefore this study aimed to analyze the clinico–epidemiological profile and survival outcome among patients presenting to kassala teaching Hospital with HC.
Methods
A total of 81 Patients aged ⩾18 years having been admitted to the outpatient clinic at kassala teaching hospital during January and through October 2017 with features suggestive of HC were enrolled in this study. The criteria proposed by the Seventh Joint National Committee were adopted for the definition of HC [7].
Definitions
Hypertensive emergency : HEs are characterized by severe elevations in the Blood Pressure complicated by evidence of progressive Target organ damage (TOD), such as (hypertensive encephalopathy, hemorrhagic and ischemic strokes, acute myocardial infarction, acute left ventricular failure with pulmonary edema, unstable angina, dissecting aortic aneurysm and acute or chronic renal insufficiency).
Hypertensive Urgency: HT-Us are those conditions associated with severe elevations in BP without evidence of end organ damage.
Hypertensive pseudocrisis: Hypertensive pseudocrisis is a condition characterized by transient elevation in BP due to any stressful event, such as migraine, vertigo, also may be a manifestation of panic disorder [7].
Detailed history was taken and proper physical examination was performed at the time of admission after signing an informed consent previously approved by the ethics research committee, kassala state. In the absence of circumstances that acceptable for signing, participation was authorized by the parents or guardians.
Diagnostic tests such as (blood for chemistry, urine analysis, lipid profile, ECG, chest X ray). Troponin was performed when acute coronary syndrome was suspected, and Brain computed tomography was done when brain damage suspected.
BP was measured using standard technique as recommended, in lying down as well as in standing position and average of three BP measurements obtained with a mercury sphygmomanometer and conducted by trained medical officer [9].
Exclusion criteria
This study excluded, hypertensive patients with pseudocrisis and those with BP <180\120 mm Hg. female patients presenting with preeclampsia and eclampsia, patients and patients <18 years of age.
Ethics
The study was conducted in confirmation of the national and international ethical guidelines for scientific research involving human beings (declaration of Helsinki) [10]. Ethical clearance of this study is obtained from the Research ethics committee at the ministry of health kassala state. Informed written consent was taken from the study subjects. The patients were managed according to the hospitals protocol for hypertension. It was clearly explained to the patients that refusing participation in the study will not affect their care and management.
Stistical analysis
Data was enter into computer data base using SPSS version 16, student t-test and chi-square test were used to compare between mean and proportions respectively, P< 0.05 was considered significant.
Results
From January to October 2017, 9900 Patients admitted to the emergency room at kassala teaching hospital. Of them 81(.81%) patients met criteria for hypertensive crisis and enrolled in this study. Their age ranging between 28 to 85 years and the mean age ±SD was 58± (12.7). Of these, 50 (61.7 %) patients were diagnosed as having HT-E, while 31 (38.3%) patients had HT-U. The majority were female 44(54.3) patients, 50 (61.7%) patients urban residents and 28 (35.8%) patients housewife. Regarding the clinical presentation, Headache was found in 60(74.1 %), Dizziness in 34(42.0 %), vomiting in 8(9.9%) and epitaxsis in 2(2.5%) (Tables 1,2).
| Table 1: Show: distribution of clinical characteristics of patients admitted with hypertensive crisis. | ||||
| variables | HC, N=81 | HT-E,N=50 | HT-U,N-31 | P |
| Headache | 60(74.1%) | 34(68.0%) | 26(83.9%) | .091 |
| Dizziness | 34(42%) | 20(40%) | 14(45.2%) | .410 |
| Vomiting | 8(9.9%) | 8(16.0%) | 0(00%) | .017 |
| Epistaxis | 10(12.3%) | 0(00%) | 10(32.2%) | <.001 |
| Chest pain | 9(11.1%) | 9(18%) | 0(00%) | .010 |
| Neurological deficits | 25(30.8%) | 25(50%) | 0(00%) | <.001 |
| Dyspnea ,yes | 18(22.2%) | 18(36%) | 0(00%) | <.001 |
| SBP | 205±(16.5) | 206±( (15.5) | 203±( (18.1) | .404 |
| DBP | 126±(11.4) | 126±(11.9) | 125±( (10.6) | .558 |
| HC: Hypertensive Crisis; SBP is systolic blood pressure on admission to Emergency room; DBP is diastolic blood pressure on admission to Emergency room.HT-E hypertensive Emergency and HTU is the hypertensive urgency. | ||||
| Table 2: Epidemiological characteristics of patients diagnosed as having hypertensive crisis HC (HT-E and HT-U). | ||||
| Variables | HC, N(81) | HU, N(31) | HE, N(50) | P |
| Age | 57.9 (12.7%) | 51.7 ± (11.6). | 61.9 ±( 11.8) | ≤.001 |
| male | 37(45.7%) | 10 (27%) | 27(.(73.0% | 0.046 |
| urban | 50(61.7%) | 21(42%) | 29(58%) | 0.262 |
| Non-governmental employee | 27(33.3%) | 4(14.8%) | 23(85.2%) | 0.003 |
| smoking | 19(23.5%) | 4(21.1%) | 15(78.9%) | 0.065 |
| Known hypertensive | 36(44.4%) | 8(22.2%) | 28(77.8%) | . .007 |
| Poor compliance | 29(35.8%) | 4(13.8%) | 25(86.2%) | 0.001 |
| Alcohol abuse | 4(4.9%) | 2(50%) | 2(50%) | . .496 |
| DM | 9(11.1%) | 2(22.2%) | 7(77.8%) | . .251 |
| Death | 13(16%) | 1(7.7%) | 12(92.3%) | . 011 |
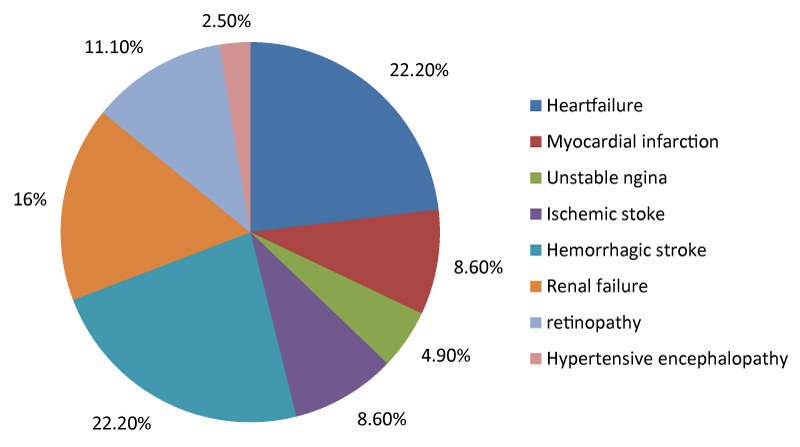
Among 50 patients who presented with features suggestive of HT-E during the study period, (Figure 1), 18(22.2%) patients had heart failure, 11(13.6%) patients had acute coronary syndrome, stroke was detected in 25(30.8% ) patients, of them 18(22.2%) patients had hemorrhagic stroke while 7(8.6%) patients had ischemic stroke, 13(16% )patients were identified to have renal failure, retinopathy was noticed in 9(11.1%) and only 2(2.5% ) patients presented with features suggestive of hypertensive encephalopathy.
Figure 1: Show; Distribution of end organ damage among fifty patients presented with HT-E, according to organ involvement.
History of smoking was found in19 (23.5%) patients, history of hypertension in 36 (44.4%) patients and history of DM was observed in 9(11.1%) patients.
Concerning the outcomes 68(84.0 %) patients discharge home while 13(16.0 %) patients died and causes of death were (stroke (9.9%) patients, ACS (2.5%) patients, renal failure (3.7%) patients).
Discussion
The main findings of this study was that the prevalence of hypertensive crisis among patients admitted to the medical emergency room at kassala teaching hospital was .81%, which is comparable to other study conducted by Carrillo et al., who reported a prevalence of HC of 0.6% among patients brought to the clinical emergency department in a Spanish university-affiliated hospital [11]. However it is inconsistent with the studies from Italy, Brazil, Bosnia and Pakistan where estimated prevalence of HC was reported as 3%,16%,47.2%and 56% respectively [1,12-14]. The difference in the prevalence rate of HC between the later studies and our result may be justified by inclusion of hypertensive pseudocrisis which may mimic hypertensive urgency, which may alter the final results of the study. AS confusion may occur in differentiating HT-U from hypertensive pseudocrisis, AS Nobre et al., have reported that 64.5% of hypertensive patients, with typical clinical manifestations of hypertensive pseudocrisis, were diagnosed incorrectly in the emergency room as having a hypertensive crisis [15].
The current study showed high prevalence of hypertensive emergency than hypertensive urgency, with approximately 2/3 of the cases corresponding to hypertensive emergency, these findings in keeping with study conducted by Manjhvar, et al. who reported hypertensive emergencies and hypertensive Urgencies as (72%) and (28%) respectively. By contrast other investigators reported high prevalence of hypertensive Urgencies [16,17].
Reasons for greater prevalence of patients with hypertensive emergency in this setting may be attributed to many reasons, like Lack of awareness about control of hypertension, poor compliance to antihypertensive drugs and inability of the poor people to have an access for healthcare may be implicated also.
Similar to other study, We found that patients with hypertensive emergencies were older, 61.9 ±( 11.8),P ≤.001 than those with HT-U. Likewise the current study demonstrated that, History of hypertension p.007, history of poor compliance to anti-hypertensive drugs p .001 and nongovernmental employee p.003 were significantly associated with HT-E [18,19].
In compare to other previously published studies, our data showed that Women had a higher frequency of hypertensive crises than men, particularly for hypertensive urgencies, this observation may be explained by greater number of women in the hypertensive population in general, also women are more sensitive of their clinical status and more frequently seek health care [18-21]. On the other hand the current study revealed that men were significantly associated with HT-E; this fact may be attributed to the differences noted in the hemodynamic status between women and men, as women, until menopause, have lower peripheral vascular resistance, hence, they have lower blood pressure levels than men at the same age. Similarly Martin et al., in his study reported high prevalence of hypertensive emergency among male [17,22].
In comparison with the study by Vilela et al., in Brazil, The present study showed that, among hypertensive emergencies, cerebrovascular accidents were the most frequent, and, among these, hemorrhagic stroke was the most common, followed by ischemic stroke, left ventricular failure, acute coronary syndrome and renal failure [23].
Regarding the clinical manifestations and according to the clinical presentation of HC the present study demonstrated that in order of frequency the clinical symptoms were headache, dizziness, neurological deficits, and dyspnea and chest pain. Such findings are in agreement with the results of many previous studies [15,24,25].
The greater case fatality rate shown in this study was comparable to that reported by many other studies [26-28].
Limitations; Firstly the sample size was small and taken from a single-tertiary care hospital, hence it represents people visiting this hospital, and not representative of the whole inhabitants.
Secondly many other risk factors like sedentary lifestyle, obesity were not considered in this study, therefore large samples size study is needed.
Thirdly retinopathy difficult to be assessed in considerable numbers of patient’s particularly very thick patients and those losing their consciousness.
Conclusion
This study showed that HT-E has high case fatality rate among patients admitted with hypertensive crisis at kassala teaching Hospital. Therefore many efforts should be directed towards early detection and appropriate management of hypertension so as to reduce morbidity and mortality among patients with hypertensive crisis.
Acknowledgement
Our thanks extended to Dr. Aurwa for his unlimited support. Also our thanks extend to staff from kassala teaching Hospital for their facilitation of the work.
References
- Salkic S, Batic-Mujanovic O, Ljuca F, Brkic S. Clinical Presentation of Hypertensive Crises in Emergency Medical Services. Materia Socio-Medica. 2014; 26: 12-16. Ref.: https://goo.gl/9KGeXB
- World Health Organization. Regional Office for Eastern Mediterranean, Clinical guideline for management of hypertension. EMRO technical publication series, Cairo 2005; Ref.: https://goo.gl/Ptet95
- Federal Ministry of Health (Sudan), World Health Organization (WHO). Sudan - Khartoum STEPS Non-communicable Disease Risk Factors Survey 2005-2006; Ref.: https://goo.gl/szBnzd
- Abdelsatir S, Al-Sofi A, Elamin S, Abu-Aisha H. The potential role of nursing students in the implementation of community-based hypertension screening programs in Sudan. Arab J Nephrol Transplant. 2013; 6: 51-54. Ref.: https://goo.gl/pdC2rE
- Federal Ministry of Health and Sudan Society of hypertension (SSH). Sudan Hypertension Guideline. Non-Communicable Diseases Directorate 2012; Ref.: https://goo.gl/kWQfLR
- Pacheco HG, Victorino NM, Urquiza JP, Castillo AA, Herrera UJ, et al. Patients With Hypertensive Crises Who Are Admitted to a Coronary Care Unit. Clinical Characteristics and Outcomes. J Clin Hypertens (Greenwich). 2013; 15: 210–214. Ref.: https://goo.gl/meULki
- Chobanian AVM Bakris GL, Black HR, Cushman WC, Green LA, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289: 2560-2572. Ref.: https://goo.gl/q5yRQe
- Sobrinho S, Correia LC, Cruz C, Santiago M, Paim AC, et al. Occurence rate and clinical predictors of hypertensive pseudocrisis in emergency room care. Arq Bras Cardiol 2007; 88: 579–584. Ref.: https://goo.gl/XApHHX
- O’Brien E, Asmar R, Beilin L, Imai Y, Mancia G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self-blood pressure measurement. J Hypertens. 2005; 23: 697–701. Ref.: https://goo.gl/y9Q92F
- World Medical Association. declaration of Helsinki .Ethical research involving Human Subjects. JAMA 2013; 310: 2191-2194. Ref.: https://goo.gl/LWrbVN
- Cerrillo MR, Hernandez PM, Pinilla CF, Claros NM, Otero ML. Hypertensive Crises: prevalence and clinical aspects. Rev Clin Esp 2002; 202: 255-258. Ref.: https://goo.gl/A4gPTK
- Zampaglione B, Pascale C, Marchisio M, Cavallo-Perin P. Hypertensive urgencies and emergencies. Prevalence and clinical presentation. Hypertension. 1996; 27: 144-147. Ref.: https://goo.gl/aSuoME
- Monteiro F, Anunciac Filhoetal F. Prevalence of true hypertensive crises and appropriateness of the medical management in patients with high blood pressure seen in a general emergency room. Arq Bras Cardiol. 2008; 90: 247–251. Ref.: https://goo.gl/9vRmQL
- Almas A, Ghouse A, Iftikhar AR, Khursheed M. Hypertensive Crisis, Burden, Management, and Outcome at a Tertiary Care Center in Karachi. International Journal of Chronic Diseases 2014; 1-7. Ref.: https://goo.gl/oZiBy7
- Nobre F, Chauchar F, Viana J, Pereira G, Lima N. Factors related to the clinical demand of a emergency service of a general and your understanding. Arq Bras Cardiol 2002; 78: 156-158.
- Al-Bannay R, Husain A. Hypertensive crisis. Clinical presentation, comorbidities and target organ involvement. Saudi Med J. 2010; 31: 916-920. Ref.: https://goo.gl/p3AGmq
- Piyanuttapull S, Angsanakul J. Prevalence of Hypertensive Emergency in Emergency Room of Rajavithi Hospital. J Hypertens Manag. 2016; 2: 1-4. Ref.: https://goo.gl/yQntCv
- Martin JF, Higashiama E, Garcia E, Luizon MR, Cipullo JP. Hypertensive crisis profile. Prevalence and clinical presentation. Arq Bras Cardiol 2004; 83: 125–130. Ref.: https://goo.gl/6ug39M
- Vilela-Martin JF, Vaz-de-Melo RO, Kuniyoshi CH, Abdo ANR, Toledo JCY. Hypertensive crisis: clinical–epidemiological profile. Hypertension Research. 2011; 34: 367–371. Ref.: https://goo.gl/BGVkDP
- Moreira GC, Cipullo JP, Martin JF, Ciorlia LA, Godoy MR, et al. Evaluation of the awareness, control and cost-effectiveness of hypertension treatment in a Brazilian city: populational study. J Hypertens. 2009; 27: 1900–1907. Ref.: https://goo.gl/nkHFRr
- Julius S. Borderline hypertension: an overview. Med Clin North Am. 1977; 61: 495-511. Ref.: https://goo.gl/qJF9GJ
- Messerli F, Garavaglia GE, Schmieder RE, Sundgaard-Riise K, Nunez BD, et al. Disparate cardiovascular findings in men and women with essential hypertension. Ann Intern Med 1987; 107: 158-161. Ref.: https://goo.gl/7QZtbm
- Vilela MJ, Érika H, Evandro G, Rizzatti LM, Paulo CJ. Hypertensive crisis profile: prevalence and clinical presentation. Arq. Bras.Cardiol. 2004; 83: 125-130. Ref.: https://goo.gl/byofSQ
- Lanthier L, Malenfant L, Lacelle MJ. Characteristics of hypertensive emergencies and urgencies at Sherbrooke between 1998 and 2006. Can J Gen Intern Med. 2008; 3: 38–40. Ref.: https://goo.gl/eLyUoA
- Serrano VC, Freites GQ, Delgado LL, García BMF. Behavior of the hypertensive crisis present in patients from NA integral diagnosis medical center. Rev Cubana Med Gen Integr. 2009; 25: 129–135. Ref.: https://goo.gl/4EriVG
- Katz JN1, Gore JM, Amin A, Anderson FA, Dasta JF, et al. Practice patterns, outcomes, and end‐organ dysfunction for patients with acute severe hypertension: the Studying the Treatment of Acute hyperTension (STAT) registry. Am Heart J. 2009; 158: 599‐606. Ref.: https://goo.gl/ND9dbL
- Badheka A, Shenoy M, Rathod A, Tuliani T, Afonso L. Long‐term mortality and role of troponin elevation in hypertensive emergencies. Am J Cardiol. 2012; 109: 600. Ref.: https://goo.gl/7gj7aw
- AlBannaya R, Husain A, Böhm M, Wagenpfeil S. Outcomes after hypertensive crisis: Comparison between diabetics and non-diabetics. IJC Metabolic & Endocrine 2015; 7: 25-30. Ref.: https://goo.gl/QyYUdC