Abstract
Research Article
Peripheral perfusion index in critically ill COVID-19 and its association with multiorgan dysfunction
Cornu Matias German*, Tonelier Matias, Roel Pedro, Sanhueza Laura, Orozco Sergio Martin, Sepulveda Mariana Elizabet, Svampa Silvana Enrica and Arana Osorio Erick and Martinuzzi Andres Luciano Nicolas
Published: 08 May, 2023 | Volume 8 - Issue 1 | Pages: 004-013
Introduction: Severe cases of COVID-19 presented a high incidence of multi-organ dysfunction syndrome (MODS) during their evolution. This was attributed to a theoretical cytokine storm, where microcirculatory disorders would play a fundamental role, causing these patients to present a sepsis-like pattern as observed in sublingual microcirculation studies. The evidence in this regard is controversial. The Peripheral Perfusion Index is a reliable method to continuously and non-invasively assess the microcirculatory bed, which assesses the pulsatile (PPI) component of the plethysmographic pulse curve.
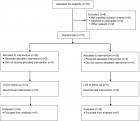
Methods: We conducted a prospective observational study to evaluate the behavior of the PPI in patients with severe respiratory failure due to SARS-CoV-2 and its association with SDOM.
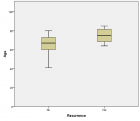
Results: We evaluated 60 patients with APACHE II 14.6 ± 4.4 and SOFA 4.7 ± 2.1. 55% of the patients presented SDOM. Perfusion monitoring showed IP values of 5.32 ± 1.87 that were associated with normal lactate levels of 1.49 mmol/L (min 0.89/ max 2.20 mmol/L). The PPI values between the living and the dead did not show a significant difference (p = 0.854) or the presence of SDOM.
The PPI values between the patients who presented renal failure, hemodynamics, or perfusion disorders were determined by the presence of hyperlactatemia, and for those who did not present these characteristics, no statistical difference was found; neither when stratified by PaFiO2 ratio. Mortality was 55%.
Conclusion: In our series of patients with severe pneumonia due to COVID-19, we found high PPI values, which would correspond to a pattern of capillary recruitment, and the associated organ injury could not be substantiated by this phenomenon.
Read Full Article HTML DOI: 10.29328/journal.jcicm.1001043 Cite this Article Read Full Article PDF
Keywords:
COVID-19; Multiorgan dysfunction; Peripheral perfusion index; Outcomes; Mortality; Critically ill
References
- Tzotzos SJ, Fischer B, Fischer H, Zeitlinger M. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Crit Care. 2020 Aug 21;24(1):516. doi: 10.1186/s13054-020-03240-7. PMID: 32825837; PMCID: PMC7441837.
- Loganathan S, Kuppusamy M, Wankhar W, Gurugubelli KR, Mahadevappa VH, Lepcha L, Choudhary AK. Angiotensin-converting enzyme 2 (ACE2): COVID 19 gate way to multiple organ failure syndromes. Respir Physiol Neurobiol. 2021 Jan;283:103548. doi: 10.1016/j.resp.2020.103548. Epub 2020 Sep 18. PMID: 32956843; PMCID: PMC7500408.
- Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and Multiorgan Response. Curr Probl Cardiol. 2020 Aug;45(8):100618. doi: 10.1016/j.cpcardiol.2020.100618. Epub 2020 Apr 28. PMID: 32439197; PMCID: PMC7187881.
- Mokhtari T, Hassani F, Ghaffari N, Ebrahimi B, Yarahmadi A, Hassanzadeh G. COVID-19 and multiorgan failure: A narrative review on potential mechanisms. J Mol Histol. 2020 Dec;51(6):613-628. doi: 10.1007/s10735-020-09915-3. Epub 2020 Oct 4. PMID: 33011887; PMCID: PMC7533045.
- Loganathan S, Kuppusamy M, Wankhar W, Gurugubelli KR, Mahadevappa VH, Lepcha L, Choudhary AK. Angiotensin-converting enzyme 2 (ACE2): COVID 19 gate way to multiple organ failure syndromes. Respir Physiol Neurobiol. 2021 Jan;283:103548. doi: 10.1016/j.resp.2020.103548. Epub 2020 Sep 18. PMID: 32956843; PMCID: PMC7500408.
- De Backer D, Donadello K, Taccone FS, Ospina-Tascon G, Salgado D, Vincent JL. Microcirculatory alterations: potential mechanisms and implications for therapy. Ann Intensive Care. 2011 Jul 19;1(1):27. doi: 10.1186/2110-5820-1-27. PMID: 21906380; PMCID: PMC3224481.
- Trzeciak S, Dellinger RP, Parrillo JE, Guglielmi M, Bajaj J, Abate NL, Arnold RC, Colilla S, Zanotti S, Hollenberg SM; Microcirculatory Alterations in Resuscitation and Shock Investigators. Early microcirculatory perfusion derangements in patients with severe sepsis and septic shock: relationship to hemodynamics, oxygen transport, and survival. Ann Emerg Med. 2007 Jan;49(1):88-98, 98.e1-2. doi: 10.1016/j.annemergmed.2006.08.021. Epub 2006 Nov 7. PMID: 17095120.
- Kanoore Edul VS, Caminos Eguillor JF, Ferrara G, Estenssoro E, Siles DSP, Cesio CE, Dubin A. Microcirculation alterations in severe COVID-19 pneumonia. J Crit Care. 2021 Feb;61:73-75. doi: 10.1016/j.jcrc.2020.10.002. Epub 2020 Oct 17. PMID: 33096349; PMCID: PMC7568145.
- Di Dedda U, Ascari A, Fantinato A, Fina D, Baryshnikova E, Ranucci M. Microcirculatory Alterations in Critically Ill Patients with COVID-19-Associated Acute Respiratory Distress Syndrome. J Clin Med. 2022 Feb 16;11(4):1032. doi: 10.3390/jcm11041032. PMID: 35207303; PMCID: PMC8876221.
- Abou-Arab O, Beyls C, Khalipha A, Guilbart M, Huette P, Malaquin S, Lecat B, Macq PY, Roger PA, Haye G, Bernasinski M, Besserve P, Soriot-Thomas S, Jounieaux V, Dupont H, Mahjoub Y. Microvascular flow alterations in critically ill COVID-19 patients: A prospective study. PLoS One. 2021 Feb 8;16(2):e0246636. doi: 10.1371/journal.pone.0246636. PMID: 33556081; PMCID: PMC7870020.
- Damiani E, Carsetti A, Casarotta E, Scorcella C, Domizi R, Adrario E, Donati A. Microvascular alterations in patients with SARS-COV-2 severe pneumonia. Ann Intensive Care. 2020 May 20;10(1):60. doi: 10.1186/s13613-020-00680-w. PMID: 32436075; PMCID: PMC7238400.
- Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020 May 2;395(10234):1417-1418. doi: 10.1016/S0140-6736(20)30937-5. Epub 2020 Apr 21. PMID: 32325026; PMCID: PMC7172722.
- Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Jonigk D. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020 Jul 9;383(2):120-128. doi: 10.1056/NEJMoa2015432. Epub 2020 May 21. PMID: 32437596; PMCID: PMC7412750.
- Jonigk D, Märkl B, Helms J. COVID-19: what the clinician should know about post-mortem findings. Intensive Care Med. 2021 Jan;47(1):86-89. doi: 10.1007/s00134-020-06302-0. Epub 2020 Nov 3. PMID: 33141245; PMCID: PMC7608308.
- Lima AP, Beelen P, Bakker J. Use of a peripheral perfusion index derived from the pulse oximetry signal as a noninvasive indicator of perfusion. Crit Care Med. 2002 Jun;30(6):1210-3. doi: 10.1097/00003246-200206000-00006. PMID: 12072670.
- Elshal MM, Hasanin AM, Mostafa M, Gamal RM. Plethysmographic Peripheral Perfusion Index: Could It Be a New Vital Sign? Front Med (Lausanne). 2021 Oct 1;8:651909. doi: 10.3389/fmed.2021.651909. PMID: 34660615; PMCID: PMC8517109.
- Rasmy I, Mohamed H, Nabil N, Abdalah S, Hasanin A, Eladawy A, Ahmed M, Mukhtar A. Evaluation of Perfusion Index as a Predictor of Vasopressor Requirement in Patients with Severe Sepsis. Shock. 2015 Dec;44(6):554-9. doi: 10.1097/SHK.0000000000000481. PMID: 26529657.
- van Paassen J, Vos JS, Hoekstra EM, Neumann KMI, Boot PC, Arbous SM. Corticosteroid use in COVID-19 patients: a systematic review and meta-analysis on clinical outcomes. Crit Care. 2020 Dec 14;24(1):696. doi: 10.1186/s13054-020-03400-9. PMID: 33317589; PMCID: PMC7735177.
- He H, Long Y, Liu D, Wang X, Zhou X. Clinical classification of tissue perfusion based on the central venous oxygen saturation and the peripheral perfusion index. Crit Care. 2015 Sep 14;19(1):330. doi: 10.1186/s13054-015-1057-8. PMID: 26369784; PMCID: PMC4568576.
- Korkut M, Bedel C, Selvi F, Zortuk O. Can peripheral perfusion index predict disease severity in COVID-19 patients in the emergency department? Ibnosina J Med Biomed Sci 2022; 14:35-40. Doi.org/10.1055/s-0042-1748776.
- Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 Mar 17;323(11):1061-1069. doi: 10.1001/jama.2020.1585. Erratum in: JAMA. 2021 Mar 16;325(11):1113. PMID: 32031570; PMCID: PMC7042881.
- Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 May;8(5):475-481. doi: 10.1016/S2213-2600(20)30079-5. Epub 2020 Feb 24. Erratum in: Lancet Respir Med. 2020 Apr;8(4):e26. PMID: 32105632; PMCID: PMC7102538.
- Hutchings SD, Watchorn J, Trovato F, Napoli S, Mujib SF, Hopkins P, McPhail M. Microcirculatory, Endothelial, and Inflammatory Responses in Critically Ill Patients With COVID-19 Are Distinct From Those Seen in Septic Shock: A Case Control Study. Shock. 2021 Jun 1;55(6):752-758. doi: 10.1097/SHK.0000000000001672. PMID: 33021572.
- Salgado DR, Ortiz JA, Favory R, Creteur J, Vincent JL, De Backer D. Microcirculatory abnormalities in patients with severe influenza A (H1N1) infection. Can J Anaesth. 2010 Oct;57(10):940-6. doi: 10.1007/s12630-010-9365-6. Epub 2010 Jul 27. PMID: 20661679; PMCID: PMC7101965.
- Fry BC, Roy TK, Secomb TW. Capillary recruitment in a theoretical model for blood flow regulation in heterogeneous microvessel networks. Physiol Rep. 2013 Aug;1(3):e00050. doi: 10.1002/phy2.50. PMID: 24040516; PMCID: PMC3770315.
- Gustafsson T, Kraus WE. Exercise-induced angiogenesis-related growth and transcription factors in skeletal muscle, and their modification in muscle pathology. Front Biosci. 2001 Jan 1;6:D75-89. doi: 10.2741/gustafss. PMID: 11145922.
- Filipovic N, Tsuda A, Lee GS, Miele LF, Lin M, Konerding MA, Mentzer SJ. Computational flow dynamics in a geometric model of intussusceptive angiogenesis. Microvasc Res. 2009 Dec;78(3):286-93. doi: 10.1016/j.mvr.2009.08.004. Epub 2009 Aug 26. PMID: 19715707; PMCID: PMC2785026.
- Ackermann M, Mentzer SJ, Kolb M, Jonigk D. Inflammation and intussusceptive angiogenesis in COVID-19: everything in and out of flow. Eur Respir J. 2020 Nov 12;56(5):2003147. doi: 10.1183/13993003.03147-2020. PMID: 33008942; PMCID: PMC7530910.
- Fernández S, Moreno-Castaño AB, Palomo M, Martinez-Sanchez J, Torramadé-Moix S, Téllez A, Ventosa H, Seguí F, Escolar G, Carreras E, Nicolás JM, Richardson E, García-Bernal D, Carlo-Stella C, Moraleda JM, Richardson PG, Díaz-Ricart M, Castro P. Distinctive Biomarker Features in the Endotheliopathy of COVID-19 and Septic Syndromes. Shock. 2022 Jan 1;57(1):95-105. doi: 10.1097/SHK.0000000000001823. PMID: 34172614; PMCID: PMC8662948.
- Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, Bolling MC, Dijkstra G, Voors AA, Osterhaus AD, van der Voort PH, Mulder DJ, van Goor H. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol. 2020 Jul;251(3):228-248. doi: 10.1002/path.5471. Epub 2020 Jun 10. PMID: 32418199; PMCID: PMC7276767.`
- Rysz S, Al-Saadi J, Sjöström A, Farm M, Campoccia Jalde F, Plattén M, Eriksson H, Klein M, Vargas-Paris R, Nyrén S, Abdula G, Ouellette R, Granberg T, Jonsson Fagerlund M, Lundberg J. COVID-19 pathophysiology may be driven by an imbalance in the renin-angiotensin-aldosterone system. Nat Commun. 2021 Apr 23;12(1):2417. doi: 10.1038/s41467-021-22713-z. PMID: 33893295; PMCID: PMC8065208.
- Karamyan VT. Between two storms, vasoactive peptides or bradykinin underlie severity of COVID-19? Physiol Rep. 2021 Mar;9(5):e14796. doi: 10.14814/phy2.14796. PMID: 33687143; PMCID: PMC7941673.
- Herrmann J, Mori V, Bates JHT, Suki B. Modeling lung perfusion abnormalities to explain early COVID-19 hypoxemia. Nat Commun. 2020 Sep 28;11(1):4883. doi: 10.1038/s41467-020-18672-6. PMID: 32985528; PMCID: PMC7522238.
- Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 Does Not Lead to a "Typical" Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2020 May 15;201(10):1299-1300. doi: 10.1164/rccm.202003-0817LE. PMID: 32228035; PMCID: PMC7233352.
- Hilty MP, Merz TM, Hefti U, Ince C, Maggiorini M, Pichler Hefti J. Recruitment of non-perfused sublingual capillaries increases microcirculatory oxygen extraction capacity throughout ascent to 7126 m. J Physiol. 2019 May;597(10):2623-2638. doi: 10.1113/JP277590. Epub 2019 Mar 28. PMID: 30843200; PMCID: PMC6826230.
- Cecconi M, Piovani D, Brunetta E, Aghemo A, Greco M, Ciccarelli M, Angelini C, Voza A, Omodei P, Vespa E, Pugliese N, Parigi TL, Folci M, Danese S, Bonovas S. Early Predictors of Clinical Deterioration in a Cohort of 239 Patients Hospitalized for Covid-19 Infection in Lombardy, Italy. J Clin Med. 2020 May 20;9(5):1548. doi: 10.3390/jcm9051548. PMID: 32443899; PMCID: PMC7290833.
- Serrano-Lorenzo P, Coya ON, López-Jimenez A, Blázquez A, Delmiro A, Lucia A, Arenas J, Martín MA; COVID-19 ’12 Octubre’ Hospital Clinical Biochemistry Study Group. Plasma LDH: A specific biomarker for lung affectation in COVID-19? Pract Lab Med. 2021 May;25:e00226. doi: 10.1016/j.plabm.2021.e00226. Epub 2021 Apr 21. PMID: 33898686; PMCID: PMC8058053.
Figures:

Figure 1
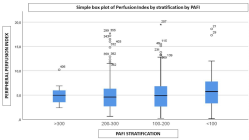
Figure 2
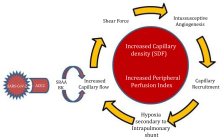
Figure 3
Similar Articles
-
Chemotherapy Exposure and outcomes of Chronic Lymphoid Leukemia PatientsJosephina G Kuiper*,Patience Musingarimi,Christoph Tapprich,Fernie JA Penning-van Beest,Maren Gaudig. Chemotherapy Exposure and outcomes of Chronic Lymphoid Leukemia Patients. . 2017 doi: 10.29328/journal.jcicm.1001006; 2: 025-033
-
Intensive Care Units (ICU): The clinical pharmacist role to improve clinical outcomes and reduce mortality rate- An undeniable functionLuisetto M*,Ghulam Rasool Mashori. Intensive Care Units (ICU): The clinical pharmacist role to improve clinical outcomes and reduce mortality rate- An undeniable function. . 2017 doi: 10.29328/journal.jcicm.1001010; 2: 049-056
-
Clinico-epidemiological characteristics and survival outcome of patients with hypertensive crisis at Kassala Hospital, Eastern SudanTajEldin M Abdallah*,Abdalazeem A Ibrahem,Ezeldein A Ali,Elbashir G Ahmed,AbdelAziem A Ali. Clinico-epidemiological characteristics and survival outcome of patients with hypertensive crisis at Kassala Hospital, Eastern Sudan. . 2018 doi: 10.29328/journal.jcicm.1001017; 3: 029-034
-
Management of Ischemic Stroke during cardiac catheterization: A case report and review of literatureNaoufal Chouaib*,Said Jidane,Mounir Lekhlit,Ahmed Belkouch,Tahir Nebhani,Saad Zidouh,Lahcen Belyamani. Management of Ischemic Stroke during cardiac catheterization: A case report and review of literature. . 2019 doi: 10.29328/journal.jcicm.1001024; 4: 040-041
-
Case reports of observed significant improvement in patients with ARDS due to COVID-19 and maximum ventilatory support after inhalation of sodium bicarbonateWardeh A*,Conklin J,Ko M. Case reports of observed significant improvement in patients with ARDS due to COVID-19 and maximum ventilatory support after inhalation of sodium bicarbonate. . 2020 doi: 10.29328/journal.jcicm.1001029; 5: 016-019
-
Effective COVID-19 prevention and control in areas of ultra-dense population: Lessons from Macau SARXueni Bian,Lan Yao,Ying Bian*. Effective COVID-19 prevention and control in areas of ultra-dense population: Lessons from Macau SAR. . 2020 doi: 10.29328/journal.jcicm.1001031; 5: 022-025
-
An educational strategy for the implementation of a delirium assessment toolBeatriz Bonaga*,Elena Ruiz-Escribano Taravilla,Carmen Carrilero-López,María Dolores Castillo-Lag,Leanne M Boehm,Ángela Prado Mira,María Joaquina Piqueras Diaz,E Wesley Ely. An educational strategy for the implementation of a delirium assessment tool. . 2021 doi: 10.29328/journal.jcicm.1001035; 6: 015-020
-
Immunocompromised patients with SARS-CoV-2 infection in intensive care units, outcome and mortalityCynthia DENIS*,Hamid MERDJI,Mathieu BALDACINI,Maleka SCHENCK,Thierry ARTZNER,Yoann GRIMAUD,Thierry LAVIGNE,Ferhat MEZIANI,Vincent CASTELAIN,Raphaël CLERE-JEHL,Francis SCHNEIDER,Guillaume MOREL. Immunocompromised patients with SARS-CoV-2 infection in intensive care units, outcome and mortality. . 2021 doi: 10.29328/journal.jcicm.1001036; 6: 021-025
-
Spinal cord involvement in tuberculous meningitis: a case report and brief review of literatureOriba Dan Langoya*,Adrian Mwota Nampogo,Andia Irene. Spinal cord involvement in tuberculous meningitis: a case report and brief review of literature. . 2022 doi: 10.29328/journal.jcicm.1001040; 7: 001-004
-
Clinical profile, etiology, outcome and new-onset diabetes: A SARI case seriesSiddharth Agarwal*,Sapna Agarwal,Raj Kumar Verma,Shreyash Dayal. Clinical profile, etiology, outcome and new-onset diabetes: A SARI case series. . 2022 doi: 10.29328/journal.jcicm.1001041; 7: 005-015
Recently Viewed
-
A Short Synthesis Concerning Biological Effects and Equivalent Doses in RadiotherapyCyril Voyant* and Daniel Julian. A Short Synthesis Concerning Biological Effects and Equivalent Doses in Radiotherapy. J Radiol Oncol. 2017: doi: 10.29328/journal.jro.1001005; 1: 039-045
-
Hepatic Angiomyolipoma Mimicking Hepatocellular Carcinoma: Another Rare Case ReportM Azzakhmam*,M Allaoui,R Elochi,A Elktaibi,M Oukabli. Hepatic Angiomyolipoma Mimicking Hepatocellular Carcinoma: Another Rare Case Report. Arch Pathol Clin Res. 2025: doi: 10.29328/journal.apcr.1001044; 9: 001-004
-
Unveiling the gut virome in human health and diseasesTao Zuo*. Unveiling the gut virome in human health and diseases. Int J Clin Virol. 2018: doi: 10.29328/journal.ijcv.1001002; 2: 001-003
-
Intrauterine Therapy with Platelet-Rich Plasma for Persistent Breeding-Induced Endometritis in Mares: A ReviewThiago Magalhães Resende*,Renata Albuquerque de Pino Maranhão,Ana Luisa Soares de Miranda,Lorenzo GTM Segabinazzi,Priscila Fantini. Intrauterine Therapy with Platelet-Rich Plasma for Persistent Breeding-Induced Endometritis in Mares: A Review. Insights Vet Sci. 2024: doi: 10.29328/journal.ivs.1001045; 8: 039-047
-
The Power of Potentized Complementary Medicines at Nanoscale for Infectious Diseases ManagementSiddharth Agarwal*,Sapna Agarwal,Shreyash Dayal. The Power of Potentized Complementary Medicines at Nanoscale for Infectious Diseases Management. J Clin Intensive Care Med. 2025: doi: 10.29328/journal.jcicm.1001054; 10: 023-030
Most Viewed
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Evaluation of In vitro and Ex vivo Models for Studying the Effectiveness of Vaginal Drug Systems in Controlling Microbe Infections: A Systematic ReviewMohammad Hossein Karami*, Majid Abdouss*, Mandana Karami. Evaluation of In vitro and Ex vivo Models for Studying the Effectiveness of Vaginal Drug Systems in Controlling Microbe Infections: A Systematic Review. Clin J Obstet Gynecol. 2023 doi: 10.29328/journal.cjog.1001151; 6: 201-215
-
Prospective Coronavirus Liver Effects: Available KnowledgeAvishek Mandal*. Prospective Coronavirus Liver Effects: Available Knowledge. Ann Clin Gastroenterol Hepatol. 2023 doi: 10.29328/journal.acgh.1001039; 7: 001-010
-
Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian RandomizationYong-Qing Zhu, Xiao-Yan Meng, Jing-Hua Yang*. Causal Link between Human Blood Metabolites and Asthma: An Investigation Using Mendelian Randomization. Arch Asthma Allergy Immunol. 2023 doi: 10.29328/journal.aaai.1001032; 7: 012-022
-
An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergiesNathalie Cottel,Aïcha Dieme,Véronique Orcel,Yannick Chantran,Mélisande Bourgoin-Heck,Jocelyne Just. An algorithm to safely manage oral food challenge in an office-based setting for children with multiple food allergies. Arch Asthma Allergy Immunol. 2021 doi: 10.29328/journal.aaai.1001027; 5: 030-037

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."